By Cindy Gaines, RN, MSN, Chief Clinical Transformation Officer, Lumeon
A perfect storm is forming in perioperative care — a crisis primed to hit very soon. It is, in short, a capacity crunch.
Staff are burnt out and quitting the profession at record rates, and recruitment of new staff is becoming a major problem. In our recent survey of 85 surgery leaders, 84% named staff burnout and retention as one of their institution’s top three short-term challenges, and 76% saw it as one of their top three long-term challenges. With such a widespread issue, action is needed to avoid patient experience, safety, and overall care suffering as a result.
Too often, when we lose staff, we lean on the rest of the team to pick up the slack. That is not going to work in this current environment. Instead of asking our teams to do the same or more with less, it is time to think about doing things differently. It is time to think about how we can make this easier for the team while providing equal or better care. There is much we can do now to improve the situation by streamlining care with the use of automation technology. Well-placed, comprehensive, digital tools can free up capacity, reduce staff burnout, and improve productivity.
How can you help your staff?
Our research surfaced several approaches to reduce burnout and retain perioperative staff, ensuring they are supported as they work to provide robust perioperative care.
Streamline surgery throughput
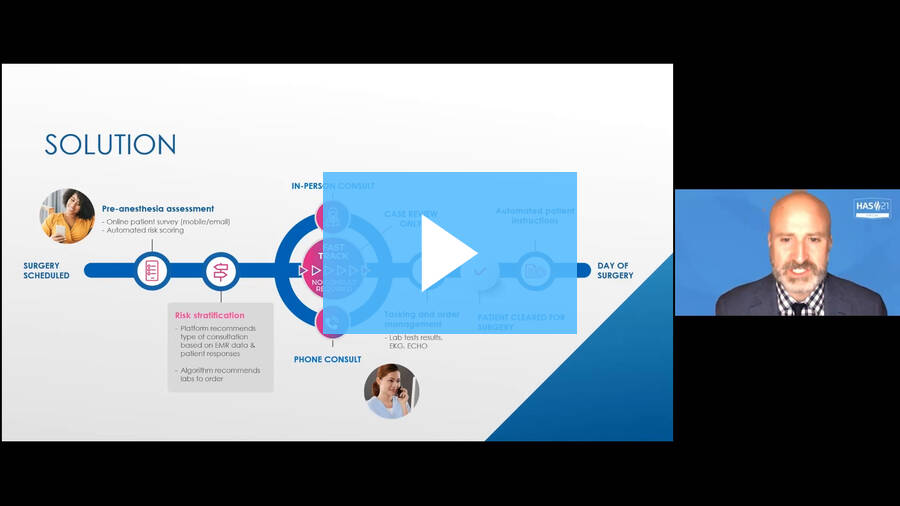
The preoperative readiness process has many manual touches to keep the patient on track. If not managed well, it can result in late surgical cancellations and scheduling/rescheduling, which then affects surgery throughput.
Nurses spend significant time cold calling patients, transcribing patient information in the medical record, chasing labs, and reaching out to communicate with pre-surgery readiness instructions to ensure the patients are ready to come in for their procedures. These activities are not only time consuming but also keep the nurse from working at the top of their license.
We can better utilize our valuable resources by streamlining the perioperative process, using automation to support patients in completing their surgical intake assessment, and discretely pushing this much-needed data into the electronic medical record. No more entering this information manually!
Combine this automation with a preoperative risk assessment calculator, and we can risk-stratify patients, identifying those who are low-risk and can be fast-tracked virtually through the preoperative process. This virtual preoperative process has been shown to increase staff efficiency by 60%.
What does this mean? It means increasing overall team capacity to see patients and allows nursing staff to spend more quality, focused time with higher-risk patients who need more attention. Staff freed up by this automation and digital engagement can spend more time working at the top of their license.
Perioperative leaders see the value in this approach, with 68% of those we surveyed saying they would prefer most of their patients to use virtual, automated preoperative readiness in the next year.
Reduce Waste
Historically, healthcare has functioned in a mode of – if we build, they will come, requiring patients to come in for face-to-face appointments. But in today’s world, there are many reasons why patients may want to avoid unnecessary in-person visits. Perhaps they have transportation challenges, cannot take time off work or secure childcare, or they are fearful of COVID exposure.
On top of this, hospitals operating with fewer staff also need to reduce time waste and risk by only bringing in patients when they need to be present in person. Almost half of the survey respondents said that healthcare organizations could save costs and reduce the burden on staff by removing unnecessary steps (49%) and removing unnecessary testing (46%). We can achieve this with automation support to help manage the preoperative process.
To learn more about how to address the capacity crunch and start improving productivity in perioperative care, download our new U.S. healthcare leadership research report, “The New Productivity Era for Perioperative Care.”

Bonus: Find out how a large IDN boosted preoperative team productivity AND achieved:
- proactively identify and screen low-risk patients
- Fast-track low-risk patients with automated engagement
- task and coordinate the preoperative team
- automate and identify gaps in care
- ensure that exactly the right care is delivered to every patient, every time