By Dan Horne, Six Sigma Business Analyst & Nefeli Kritikou, Marketing Manager, Lumeon
Engaging with patients and their families is a necessity for clinicians, given its benefits on clinical outcomes and healthcare sustainability. Patient engagement not only raises patients’ satisfaction and psychological well-being but also reduces medical errors and improves overall medical safety.
While doctor-patient communication is a key determinant in adherence to many care plans, the importance of surgeon-patient communication is amplified by the invasiveness, risk, and complexity of surgical procedures. Given the prolonged time from admission to full recovery, surgeons are required to engage with their patients from the very beginning of their care relationship. This ensures that patients will remain engaged throughout the surgery experience and in the follow-up phases of their care pathway.
Focusing on early patient engagement is particularly crucial for Enhanced Recovery After Surgery (ERAS®), a multidisciplinary and multimodal evidence-based improvement process to the care of the surgical patient. Our last blog explained how health teams can implement ERAS® protocols preoperatively, to achieve improved outcomes. In this post, we will focus on postoperative patient engagement, and show how it can be optimized by implementing ERAS protocols and more.
Why you should optimize postoperative patient engagement
While in previous years, the surgery experience was solely focused around the procedure and its clinical outcomes, nowadays this focus has opened up to a broader consideration of the psychosocial components of the illness experience (1). This recent focus on the potential impact of surgery on patients’ lifestyles and attitudes on their medical adherence has underlined the importance of postoperative patient engagement (2). From the patient’s perspective, enhanced participation and on-going engagement in their post-surgery journey is necessary in order to regulate their emotions, understand and follow advice and achieve an overall better alignment of their treatment to their psychological experience and needs (3).
Psychosocial Patient Support
Patients and caregivers efforts with the various post-operative duties, however, they can often feel not adequately equipped at an informative and emotional level (3). Committed healthcare systems focus on post-operative patient engagement to sustain patients and their family health literacy and equip them with the needed skills for the effective self-management of their recovery (4,5). Patients who feel that they have a strong relationship with their doctors, surgeons and medical professionals are more likely to be satisfied with their care, share information pertinent to their recovery, adhere to the prescribed treatment plans and even make referrals to friends.
Medical Outcomes
Two-way patient communication can also help health teams identify patients who are at risk of medication non-adherence and take steps to encourage adherence and mitigate risk behaviors. Research also reveals that surgeon-patient communication is critical in mitigating and managing postoperative complications (6). In fact, patient engagement is identified as being more predictive of treatment adherence than satisfaction from the surgical outcomes. As engaged patients are more likely to communicate health status changes or recovery threats to their doctors, the clinical team has the opportunity to timely intervene and prevent complications or readmissions.
Postoperative engagement through ERAS®
The Enhanced Recovery After Surgery (ERAS®) programme applies evidence-based perioperative protocols that improve patient recovery and reduce the length of hospital stay (7-9), by focusing on analgesia, mobilization, and discharge. ERAS protocols assemble several care elements, which form a care pathway that engages everyone involved in the care of the patient (10). This post-operative engagement and support along with patients’ psychological resilience and sense of ownership are extremely important for the physiological outcomes of the intervention (11). Patients are in general more likely to assume a proactive and participative role until the stage of full recovery when they are part of a consistently engaging care environment.
Where is the problem then?
Despite the robust evidence in favor of compliance with ERAS®, implementing ERAS® is a challenging task. Care teams face a number of institutional barriers, such as the lack of nursing staff and financial resources, as well as poor communication and collaboration within the team (12). Even when these barriers are overcome, it is unsure whether high levels of compliance can be sustained in the long-term. Studies have shown that non-compliance is even more likely in the post-operative period, where different groups of professionals are involved, each with varied priorities (13). The lack of a standardized, consistent implementation process for ERAS® significantly affects the performance of the care team.
Patient participation is also particularly difficult post-operatively, given patients’ acute psychological stress, which can impede understanding and retaining medical advice (14). Studies have shown that post-operative information related to explaining pain management and the care pathway needs to be repeated several times during the follow-up period until patients achieve full recovery (15). However, as they predominantly focus on reducing the length of hospital stay, ERAS protocols currently offer no further recommendations for the follow-up period at home. This affects the adherence rate to the ERAS approach, which has been proven to be lower in the postoperative phase (16).
At the same time, and while researchers are reporting an overall high level of contentment with the implementation of ERAS protocols, postoperative support has been consistently documented as not meeting the patient needs (17-20). Research has shown that patients believe that ERAS programmes should not be limited to the perioperative period, but should encompass the entire journey from diagnosis to recovery (21). As healthcare organizations now value patient satisfaction as much as patient safety and clinical workflow improvements (22), the need for an operationally integrated pathway enabling them to go beyond ERAS® is made clear.
Going beyond ERAS®
by Dan Horne, Six Sigma Business Analyst, Lumeon
ERAS® aims to offer a structured approach to postoperative patient management. This recovery approach mainly covers the area of early mobilization – given that prolonged immobilization has proven to increase the risk of pneumonia, insulin resistance and muscle weakness, and the prevention of postoperative ileus, through urinary drainage, postoperative analgesia advice, and postoperative glucose control.
ERAS® has also introduced the completion of patient diaries or journals prior to discharge, which has allowed medical staff to have an early insight into how the patient feels and their rate of recovery. Patient recovery is measured against a set of daily goals over the days in which they are hospitalized, following surgery and prior to discharge.
These activities are beneficial and undoubtedly help reduce length of stay, whilst simultaneously involve the patient, family member and carers in the recovery process. However, this best in class advice on enhanced patient recovery is often difficult to be implemented by the care teams and stops following the patient being discharged. Given the financial implications around readmissions within the first 30 days following surgery, it is necessary to ensure that patients, not only recover quickly but also do not relapse leading to costly readmissions. Care teams, therefore, need to follow a consistent standardized process to implement ERAS® protocols during hospitalization and take additional steps in the follow-up period at home.
Enhanced patient communication and education following hospital discharge can ensure that the patient is ‘on track’ and is following postoperative advice – such as adhering to the medication protocol, exercising, eating and drinking correctly. Patient support networks can be involved and family members or carers can also actively participate in the activities that will ensure a rapid recovery with minimal complications. To achieve these, care teams need to extend patient engagement to the period patients are recovering at home, through a fully automated pathway integrated with the systems they already use.
Lumeon’s Care Pathway Manager allows a seamless end to end communication customizable between care providers and patients. Patient journals, PROMs (Patient Reported Outcome Measurements), educational material and more can be distributed to the patient using their preferred communication method. Intelligent algorithms can evaluate patient responses to check that the patient is recovering as expected. In the case of receiving adverse results from any of the patients’ responses, our system can risk stratify the patient and trigger an automated escalation for those who are not recovering as expected. These patients can be changed to high touch pathways – either requesting further patient information or placing them on a call list for follow up by medical staff.
In addition to early notification of potentially adverse events, the frequent communication between medical organizations and the patient or family members ensures that the patient feels that the care provider shows an active interest in their wellbeing which leads to increased patient satisfaction and positive feedback. With no limitations on the recall time period or the number of communications that can be sent out to the patient, our CPM ensures ongoing efficient communication and patient engagement that both enables and goes beyond ERAS® postoperative protocols.
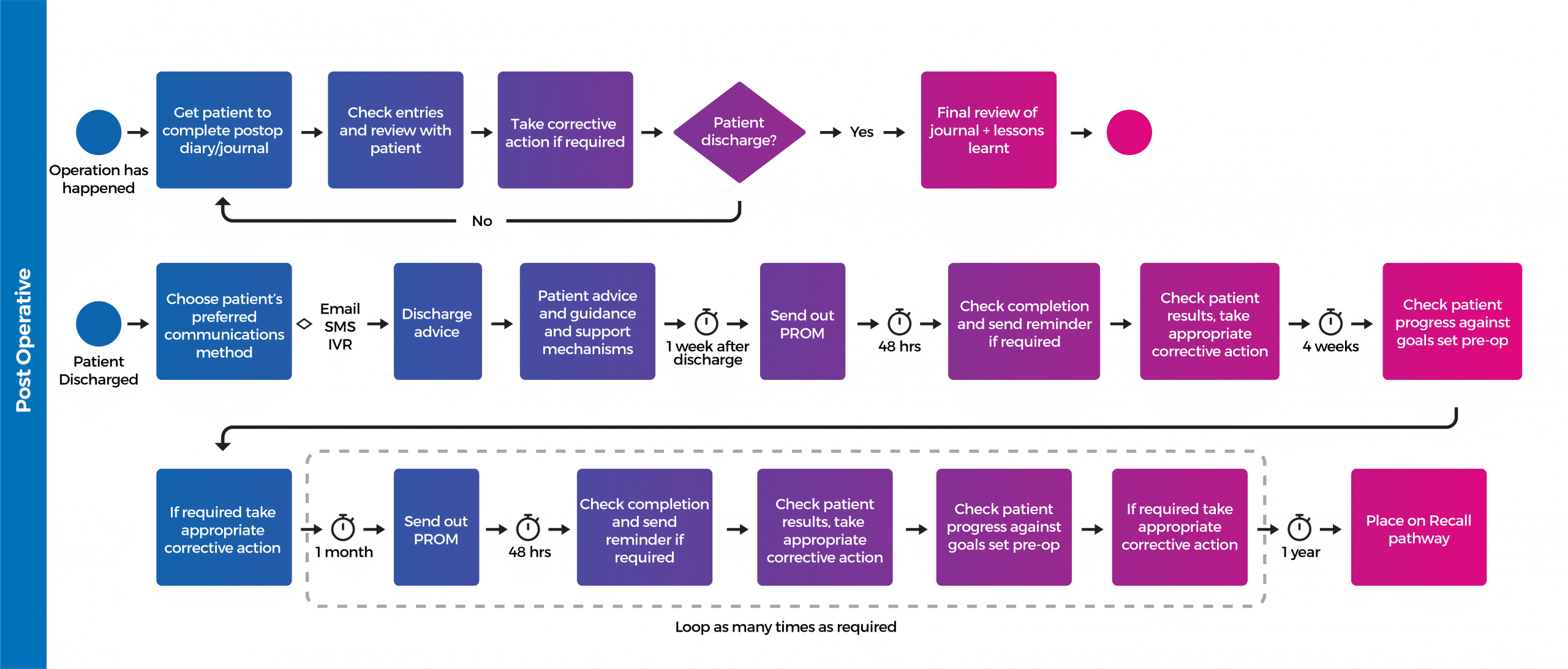
A typical post-discharge communication pathway is shown below, though CPM is able to tailor it’s solution exactly to the needs of the care provider. Click on the image to view full size.
Conclusion
Sustaining patient engagement in the surgery experience is a crucial predictor of the quality of patients’ psychological and medical outcome. The success of the ERAS® approach is not only dependent on treatment management innovations, but also on the ability of the surgery team to engage patients in becoming more participative throughout their experience. Engaged patients feel better prepared to continue their recovery at home, which leads to reduced length of hospital stays and improved healthcare financial outcomes. However, the ERAS® approach is difficult to implement and currently stops at the time of discharge, which leads to preventable readmissions and patients complaints for inadequate postoperative support. Going beyond ERAS® is necessary for health organizations looking to improve patient satisfaction and prevent financial implications.
Interested in finding out more about care pathway management for Surgery?
REFERENCES
- 1. Beisecker, AE. Beisecker, TD. Using Metaphors to Characterize Doctor–Patient Relationships: Paternalism Versus Consumerism.Health Commun 1993;5:41-58. 10.1207/s15327027hc0501_3
- 2. Taylor, K. Paternalism, participation and partnership – the evolution of patient centeredness in the consultation. Patient Educ Couns. 2009 Feb; 74(2):150-5.
- 3. Martin, LT. Schonlau, M. Haas, A. et al. Patient activation and advocacy: which literacy skills matter most? J Health Commun 2011; 16 Suppl 3:177-90. 10.1080/10810730.2011.604705
- 4. Weinberger, SE. Johnson, BH. Ness, DL. Patient- and family-centered medical education: the next revolution in medical education? Ann Intern Med. 2014 Jul 1; 161(1):73-5.
- 5. Carman, KL. Dardess, P. Maurer, M. et al. Patient and family engagement: a framework for understanding the elements and developing interventions and policies. Health Aff (Millwood). 2013 Feb; 32(2):223-31.
- 6. Messano, GA. Spaziani, E. Turchetta, F. et al. Risk management in surgery. Il Giornale di Chirurgia. 2013;34(7-8):231-237.
- 7. Ljungqvist, O. Scott, M. Fearon, KC. Enhanced recovery after surgery: a review. JAMA Surg 2017;152:292-298. Epub ahead of print.doi:10.1001/jamasurg.2016.4952
- 8. Nelson, G. Kiyang, LN. Crumley, ET. et al. Implementation of Enhanced Recovery After Surgery (ERAS) Across a Provincial Healthcare System: The ERAS Alberta Colorectal Surgery Experience. World J Surg 2016;40:1092–103.doi:10.1007/s00268-016-3472-7
- 9. Nguyen, T. Chuck, A. Wasylak, T. et al. An economic evaluation of the enhanced Recovery after Surgery (ERAS) multi-site implementation program for colorectal surgery in Alberta. Can J Surg 2016;59:6716
- 10. Ljungqvist, O. Hubner, M. Enhanced recovery after surgery—ERAS—principles, practice and feasibility in the elderly. Aging Clinical and Experimental Research. 2018;30(3):249-252. doi:10.1007/s40520-018-0905-1.
- 11. Haskell, H. Lord, T. Patients and Families as Coproducers of Safe and Reliable Outcomes. In: Sanchez J, Barach P, Johnson JK, et al. editors. Surgical Patient Care: Improving Safety, Quality and Value. Cham: Springer International Publishing, 2017:101-20.
- 12. Pearsall, EA. Meghji, Z. Pitzul, KB. Aarts, M-A. McKenzie, M. McLeod, RS. et al. A qualitative study to understand the barriers and enablers in implementing an enhanced recovery after surgery program. Ann Surg. 2015;261:92–6.
- 13. Kohokeh, A. Sammour, T. Zargar Shoshtari, K. et al. Implementation of ERAS and how to overcome the barriers, International Journal of Surgery https://doi.org/10.1016/j.ijsu.2008.11.004
- 14. Kessels, RP. Patients’ memory for medical information. J R Soc Med 2003;96:219-22.
- 15. Sjöstedt, L. Hellström, R. Stomberg, MW. Patients’ need for information prior to colonic surgery. Gastroenterol Nurs 2011;34:390-7.
- 16. Ankit, S. (2016) ‘Implementing Enhanced Recovery After Surgery’ [PowerPoint Presentation] Available at https://www.hasc.org/sites/main/files/sarin_implementing_eras_-_060916.pdf (Assessed 11 September, 2018)
- 17. Blazeby, JM. Soulsby, M. Winstone, K. et al . A qualitative evaluation of patients’ experiences of an enhanced recovery programme for colorectal cancer. Colorectal Dis 2010;12:e236–e242.doi:10.1111/j.1463-1318.2009.02104.x
- 18. Bernard, H. Foss, M. Patient experiences of enhanced recovery after surgery (ERAS). Br J Nurs 2014;23:100–6.doi:10.12968/bjon.2014.23.2.100
- 19. Aasa, A. Hovbäck, M. Berterö, CM. The importance of preoperative information for patient participation in colorectal surgery care. J Clin Nurs 2013;22:1604–12.doi:10.1111/jocn.12110
- 20. Sibbern, T. Bull Sellevold, V. Steindal, SA. et al. Patients’ experiences of enhanced recovery after surgery: a systematic review of qualitative studies. J Clin Nurs 2017;26. Epub ahead of print.doi:10.1111/jocn.13456
- 21. Gillis, C. Gill, M. Marlett, N. et al Patients as partners in Enhanced Recovery After Surgery: A qualitative patient-led study BMJ Open 2017;7:e017002. doi: 10.1136/bmjopen-2017-017002
- 22. Heath, S. (2016) ‘Patient Satisfaction Becomes Critical Concern for Hospitals’ Patient Engagement HIT, 4 May Available at: https://patientengagementhit.com/news/patient-satisfaction-becomes-critical-concern-for-hospitals (Assessed 11 September, 2018)